
Are Your Nurses Leaving by the Droves? (Or wanting to?)
There could be several reasons why your nurses are leaving your facility or talking about looking for work elsewhere. Maybe you, too, have started wondering if the grass is greener at some other place or in some other role.
Georgia could see the largest shortage of registered nurses by 2036, with an estimated 34,800 vacancies, according to a recent report from the Health Resources and Services Administration. Is your state listed in the top 10 affected by RN shortages?
A primary cause of nurses resigning or taking positions at other hospitals is the chronic underfunding of the healthcare system. Many nurses start their careers because they love medicine and helping people, and they often dedicate a ton of their time and effort to improving the system. However, some veteran nurses eventually decide that the current system can’t be fixed and their only option is to leave.
Many medical practices and hospital systems have recognized there is a problem and have even sought ways to create financial sustainability, but some of those decisions can create tension among staff and lead to internal conflicts that exacerbate the issues rather than solve them.
The best solution is one that balances financial obligations, operational best practices, federal and state board regulations, and the finest medical care. While there is an accepted Fundamental Framework of Care that can help nurses level-set expectations and navigate the system, without such a framework in place, nurses will continue to leave in droves.
Why Some Nurses Are Leaving to Become Travel Nurses
Nurses are increasingly leaving their employment at a single local hospital to become travel nurses for several key reasons:
Sign up to get the latest industry news and offers right in your inbox
- Higher Pay: Travel nursing typically offers significantly higher pay compared to permanent hospital positions. This includes not only higher hourly rates but also bonuses, stipends for housing, and travel reimbursements.
- Flexibility and Freedom: Travel nurses have more control over their schedules and can choose assignments that fit their personal lives. They can take time off between assignments, which offers more flexibility than a traditional hospital job.
- Work-Life Balance: The ability to choose assignments and locations allows travel nurses to achieve a better work-life balance. They can avoid burnout by taking breaks when needed and by selecting locations that might be more desirable or closer to family.
Read More: “Exploring Travel Nursing: What Is a Travel Nurse, And How Do You Become One?”
- Experience and Adventure: Travel nursing offers the opportunity to work in different hospitals across the country, allowing nurses to gain a wide range of experiences. This variety can be appealing to those who want to avoid the monotony of working in the same place every day.
- Work Environment: Some nurses leave permanent hospital positions due to dissatisfaction with their work environment, including understaffing, high patient loads, and lack of support. Travel nursing can offer a change in environment and, in some cases, a better work setting.
- Pandemic-Driven Demand: The COVID-19 pandemic created a surge in demand for travel nurses, leading to increased pay and opportunities. Many nurses found the compensation and the chance to contribute to critical care needs during the pandemic compelling and have remained as travel nurses to crisis locations for the meaningful purpose it provides.
- Burnout: Hospital nursing can be physically and emotionally draining, especially in high-pressure environments. The flexibility and higher pay of travel nursing can make it a more attractive option for those experiencing burnout in permanent positions.
These factors combine to make travel nursing an appealing alternative to traditional hospital employment for many nurses. For those who want to remain where they are and are seeking support or ways to improve their environment, keep reading.
What Are the Fundamentals of Care Framework?
A recent article by Susan Mace Weeks highlights the importance of engaging nurses and placing patients at the center of care.
However, Meeks recognizes that nurses do not work in a world of their making and are instead beholden to the larger systems that dictate policy and procedure. While nursing is the science and art of promoting positive human responses to health and illness, and the foundation for being an effective nurse is the ability to develop a professional-yet-amiable relationship with patients, nurses are all too aware that system design and healthcare policy can either support or impede delivery of care.
The Fundamentals of Care Framework, created and promoted by the International Learning Collaborative (ILC), “provides a pragmatic conceptualization of nursing and creates a structure to organize work within practice, educational, and policy settings. The framework also provides abundant opportunities to support the advancement of nurses’ knowledge base and outcomes in the areas of evidence-based practice, quality improvement, and research.”
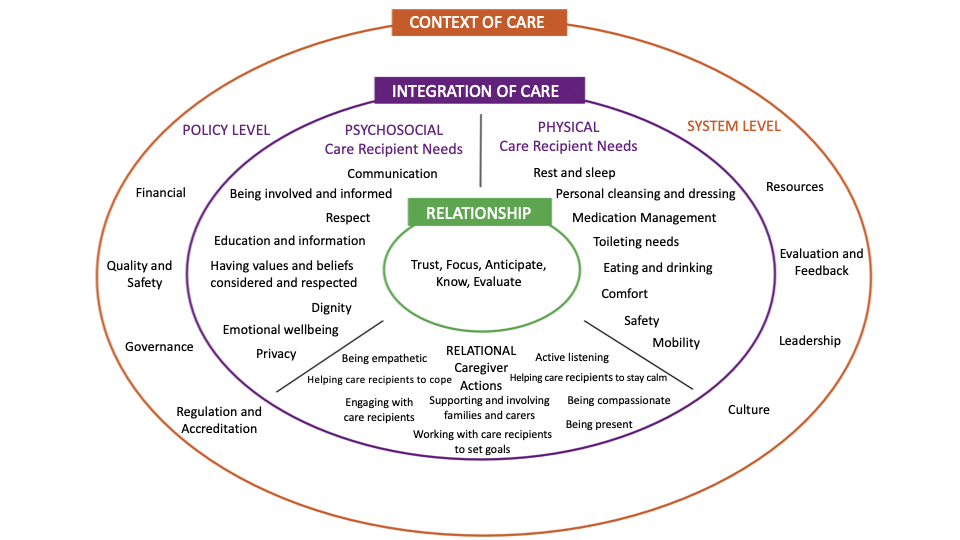
Image obtained from ilccare.org/the-fundamentals-of-care-framework/ Content within image derived from 1) Kitson, A., Conroy, T., Kuluski, K., Locock, L., & Lyons, R. (2013). Reclaiming and Redefining the Fundamentals of Care: Nursing’s Response to Meeting Patients’ Basic Human Needs. School of Nursing, The University of Adelaide, Adelaide, South Australia. digital.library.adelaide.edu.au/dspace/bitstream/2440/75843/1/hdl_75843.pdf; and 2) Feo, R., Conroy, T., Jangland. E., Muntlin Athlin, Å., Brovall, M., Parr, J., Blomberg, K., & Kitson, A. (2017). Towards a standardized definition for fundamental care: A modified Delphi study. Journal of Clinical Nursing, 27, 2285-2299. doi: 10.1111/jocn.14247
Implementing the Fundamentals of Care Framework
The 2013 report published by The University of Adelaide was key in creating the framework for nursings’ current Fundamentals of Care.
The report emphasizes the importance of creating optimal working environments for nurses by focusing on the Fundamentals of Care (FOC) and patient-centered care (PCC). It highlights the need for nurses and clinicians to articulate the significance of FOC work, linking it to organizational KPIs and quality agendas.
Stressing the importance of defining the role of nursing within healthcare facilities, the report encourages executives to identify the impact of each nursing role on patient care, create detailed and specific job descriptions, and refine recruitment and selection processes to prioritize the delivery of FOC.
Additionally, the publication underscores the development of integrated roles that facilitate effective FOC delivery, the enhancement of nurses’ critical thinking approaches, and the implementation of tools and measures to assess the impact of FOC delivery.
Of course, nursing best practices don’t start at the hospital. Educators must do better to integrate FOC into nursing curricula, exploring mentorship roles and the use of clinical simulation to enhance PCC delivery.
Having the right physical and human resources, a supportive organizational culture that values PCC, effective leadership styles, and mechanisms for continuous evaluation and feedback are crucial for creating optimal working environments for nurses and enhancing the quality of care provided by nurses.
This seminal 2013 report was published in Australia, and while some North American practitioners value and prioritize the Fundamentals of Care, others tend to refer to fundamental care classes and related texts as “Fundamentals of Nursing,” focusing more on foundational nursing skills and early practice experiences.
This discrepancy raises questions about the perceived simplicity of fundamental care tasks versus the very real challenges nurses currently face in consistently delivering high-quality, personalized care.
What Makes Champion Different From Competitors?
We agree with putting patients at the center of care, but we also engineer our medical seating with nurses in mind.
Read More: “Designing Medical Chairs With Caregiver Ergonomics in Mind”
At Champion, we believe that comfort, safety, functionality, and ease of access isn’t just for patients: It’s for providers and caregivers too.
That’s why our products — whether medical recliners, clinical essentials, or procedure chairs — are the best option for your facility.
To view our entire portfolio of medical seating, fabrics, and accessories, browse our digital catalog. Then, request a quote for your facility today.
