How to Prevent Hospital-Acquired Infections in Your Facility
The longer a patient stays in a hospital or healthcare facility of any kind, the greater their risk of contracting a hospital-acquired infection, also called a hospital-associated infection (HAI).
HAIs are infections that patients develop while staying in a medical facility, which weren’t present (or even incubating without symptoms) when they were admitted. Symptoms of infection tend to manifest around 48 hours after admission.
These infections are often linked to medical devices and procedures, posing a risk to patient safety. Some common examples include infections from catheters, central lines, surgeries, ventilators, and pneumonia — as well as infections like Clostridium difficile (commonly referred to as C. diff).
Signs of these infections can include a variety of symptoms, such as a productive cough, shortness of breath, abdominal pain, and confusion. The focus for medical providers is on how to evaluate and manage these infections — and the importance of a team approach in providing the best care for patients affected by them. The focus of this blog is on ways to prevent the HAIs from occurring in the first place.
For healthcare workers wanting to do more research on this subject, a recent NCBI report discusses the significant challenge of hospital-acquired infections. The report outlines various pathogens responsible for HAIs, including bacteria, viruses, and fungi, and emphasizes the importance of strict infection control practices to prevent their spread. The report also highlights the critical need for ongoing surveillance, education, and adherence to guidelines to reduce the incidence of HAIs and protect patient health.
Sign up to get the latest industry news and offers right in your inbox
How to Prevent HAIs From Occurring
The most common (and quite easy) prevention strategies include hand hygiene, the use of personal protective equipment, and environmental cleaning. When it comes to environmental cleaning, the Centers for Disease Control and Prevention (CDC) provides detailed guidelines on how to control infections in healthcare facilities.
However, even with relatively healthy patients, inadvertent exposures to environmental pathogens or airborne pathogens can result in adverse patient outcomes and cause illness — among healthcare workers too. These incidents of Healthcare Acquired Infection can be minimized by appropriate use of cleaners and disinfectants and the use of quality medical equipment that is properly maintained.
Medical equipment should be inspected, checked, and tested regularly to ensure it is safe and operating effectively. Many federal and state regulatory agencies such as the FDA and OSHA require annual inspections of all medical equipment that comes in contact with patients in order to prevent injury or misdiagnosis.
There are also routine hygiene practices, plus cleanings after spills or contact with bodily fluids, and also deep cleanings that remove product parts in order to access areas typically out of reach.
Elevator buttons, stair rails, counter surfaces, door, drawer, and cabinet handles, light switches, phones, keyboards, and computer mice should be disinfected every day. It’s also recommended to clean them between patient contact. Because this requires repeated work, some people want to save time and effort by using disinfectant wipes. But do wipes kill viruses?
Generally, because disinfectant wipes have shorter dwell times than most disinfectant chemicals, they may not have enough time to kill the viruses on a surface. The CDC advises using disinfectant wipes that contain at least 60% alcohol to target viruses like the norovirus, influenza, rhinovirus, and coronavirus.
The Best Medical Chair Fabric for Antimicrobial Protection
The coverings on medical seating do more than protect the life of the equipment; they can also help protect the life of the patient.
With nearly a billion Americans visiting a doctor’s office each year, you can imagine the number of “touches” each chair and piece of medical seating receives. With so many people sitting in, touching, and variously using the products, it’s easy to understand why keeping the item clean is so important. In fact, there are laws that demand it.
If medical seating coverings are so important, the question becomes, What do I need to look for when buying products for my healthcare facility? For starters, fabrics need to be durable because torn materials can’t be easily cleaned. Porous fabrics are more likely to absorb bodily fluids.
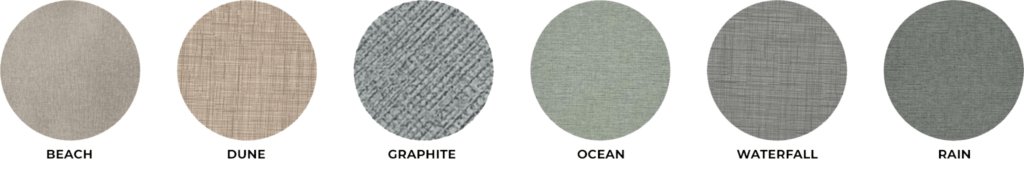
Champion’s Secura performance covering supports the harsh demands of healthcare, while offering the welcoming appearance of a textile.
Details Facility Directors Care About — Secura Fabrics Are:
- 100% Polyurethane
- Graffiti-Free Finish
- PFAS-Free
- PVC-Free
- Superior Hydrolysis
- 500,000 Double Rubs
- Bleach Cleanable
- No Harmful Chemicals
- Zero Plasticizers
- 6 Colors Available
- Passed — AAMI TIR12
- Passed — AAMI ST98
- Passed — AATCC147
- Passed — ISO 17664
With Secura, medical professionals can decrease the risks for healthcare-associated infections while also increasing patient comfort. What’s more — the facility boasts an attractive, modern look that meets the needs of staff, patients, and the bottom line.
To view our entire portfolio of medical seating, fabrics, and accessories, browse our digital catalog. Then, request a quote for your facility today.
