As of August 2025, labor and delivery services across the United States are facing unprecedented strain. The crisis is especially acute in rural areas, where entire counties have lost maternity wards, leaving thousands of families without local access to safe childbirth.
For many expectant mothers, what should be a moment of joy is instead clouded by uncertainty: Will I make it to the hospital in time? What happens if there’s an emergency? These are not hypothetical questions—they’re daily realities in communities across the U.S.
Widespread Closures of Rural Maternity Units
Since 2020, more than 100 rural hospitals have shuttered their labor and delivery units, and fewer than 1,000 remain nationwide. This wave of closures has created what experts call “maternity care deserts”—regions where no hospital offers obstetric services.
- In Alabama, nearly one-third of rural hospitals have stopped delivering babies (CHQPR Rural Maternity Care Crisis).
- In Texas, nearly half of all counties—about 46%—lack hospital-based obstetric care (March of Dimes).
- In many rural regions, closures mean far longer drives to reach care, often at least 30 minutes and sometimes 50 minutes or more (CHQPR Rural Maternity Care Crisis).
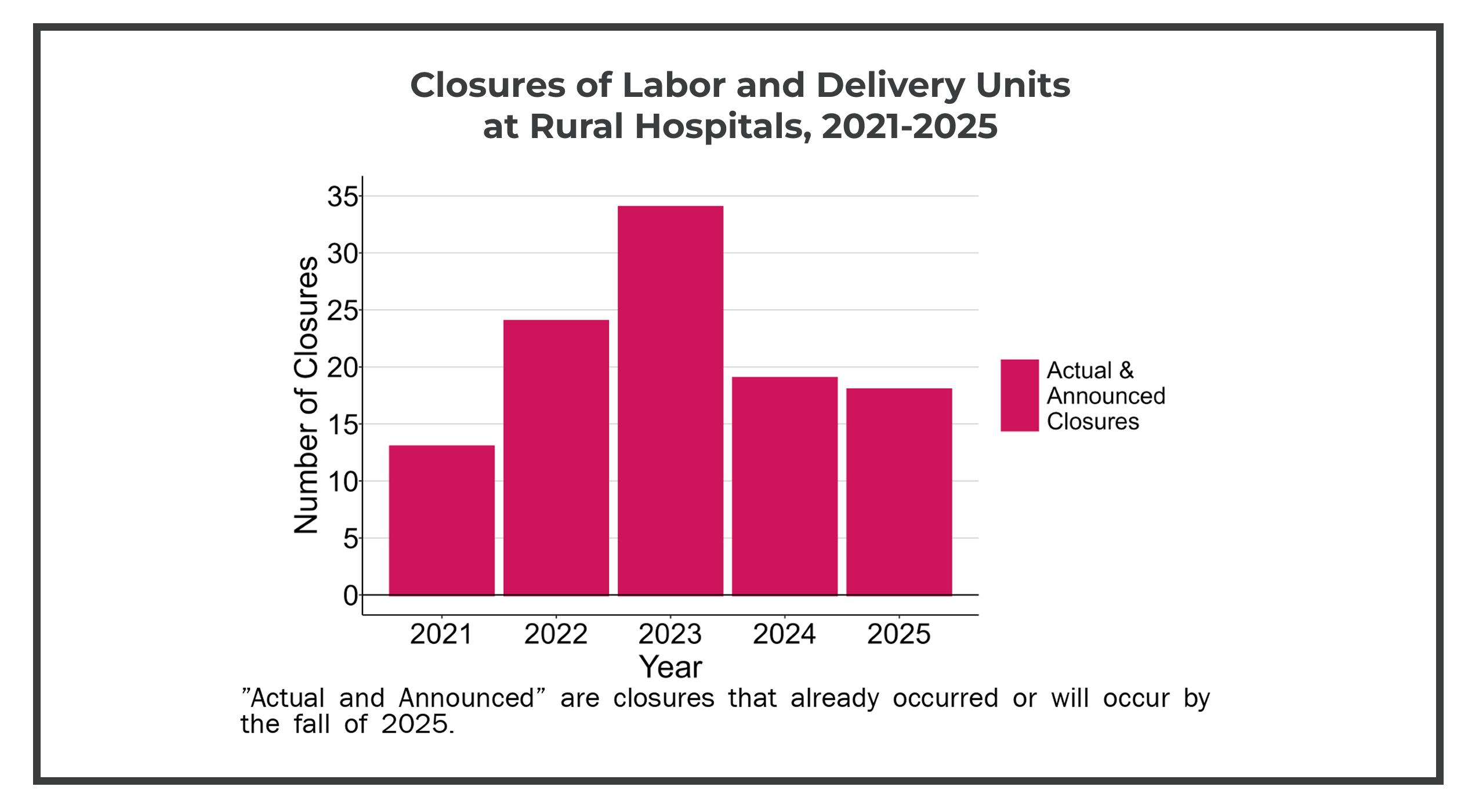
These closures aren’t just numbers. They represent lost lifelines in communities where alternatives are few and far between.
Sign up to get the latest industry news and offers right in your inbox
Why Labor and Delivery Units Are Closing
The forces behind this trend are interconnected and complex:
1. Financial Constraints
- Medicaid pays for over 40% of births in the U.S., but in rural areas, reimbursement rates are often below cost.
- Labor and delivery units require specialized staff and 24/7 readiness, which is expensive when patient volumes are low.
2. Workforce Shortages
- Recruiting obstetricians, anesthesiologists, and labor nurses to rural communities is increasingly difficult.
- Providers face long on-call shifts and limited backup, leading to burnout and turnover.
3. Declining Birth Rates
- National fertility rates have dropped steadily since the early 2000s.
- Fewer births mean fewer hospital admissions, making maternity units financially vulnerable.
When all three pressures combine, maternity services are often the first on the chopping block.
The Human Cost of Maternity Ward Closures
Longer Travel Means Higher Risks
When women must travel long distances to reach a hospital with labor and delivery services, the risks increase significantly. Delays in receiving timely care can turn otherwise manageable complications—such as preeclampsia, prolonged labor, or postpartum hemorrhage—into life-threatening emergencies.
Research consistently shows that access to care within a short travel window is critical for safe outcomes. In maternity care deserts, where families face 30 minutes or more on the road, the likelihood of giving birth outside a hospital setting—or arriving too late for immediate intervention—rises sharply. These challenges don’t just end at delivery: longer travel distances also discourage mothers from attending vital postpartum checkups, putting both maternal and infant health at risk.

Emotional and Financial Strain on Families
Families are forced to make tough decisions:
- Paying for hotels near urban hospitals as due dates approach.
- Missing work to attend long-distance prenatal checkups.
- Struggling to find childcare for older children.
These burdens weigh especially heavily on low-income families without reliable transportation.
Postpartum Care Gaps
Postpartum follow-ups are crucial for detecting complications such as blood clots, infection, or postpartum depression. Yet many mothers skip visits due to travel barriers. For infants, missed well-baby checks can delay the detection of developmental or feeding issues.
The U.S. already has the highest maternal mortality rate among wealthy nations—nearly three times that of Canada and the U.K. (Live Science). Without intervention, that gap will only grow.
Policy Solutions to the Maternity Care Crisis
Healthcare leaders and policymakers are working to stabilize maternal health access. Current proposals include:
- Medicaid Expansion & Reimbursement Reform: Ensuring rural hospitals receive payments that reflect the true cost of delivery.
- Incentives for Rural Providers: Loan forgiveness, signing bonuses, and housing stipends for obstetric staff who practice in underserved areas.
- Federal Grants for Obstetric Deserts: Funding to establish maternity clinics, birthing centers, and telehealth programs in counties with no services.
- Global Budget Models: States like Pennsylvania are piloting hospital funding models that guarantee revenue regardless of patient volume, helping hospitals keep maternity units open.
Community and Healthcare Innovations

Rural communities aren’t waiting for policy change—they’re building creative models of care:
- Mobile Maternal Health Units: Vans equipped for prenatal and postpartum care travel to remote communities weekly.
- Telehealth Obstetrics: Virtual consultations with maternal-fetal medicine specialists are becoming standard for high-risk pregnancies.
- Midwife Integration: Certified nurse-midwives are filling gaps in areas without OB-GYNs, often working in partnership with regional hospitals.
- Hospital Collaborations: Smaller facilities partner with urban medical centers to share staff rotations and patient transfers.
These initiatives are not perfect, but they demonstrate how innovation can bridge gaps in maternity care access.
FAQs on Rural Hospital Closures and Maternal Health
Why are rural maternity units shutting down?
Rising costs, low Medicaid reimbursement, and staff shortages make it hard for rural hospitals to keep labor and delivery units open—especially where birth rates are low.
What does a maternity care desert mean for families?
Families face longer travel for prenatal care, higher risks in emergencies, and fewer postpartum visits, adding both medical and financial strain.
What policies could improve rural maternity care?
Higher Medicaid reimbursement, loan forgiveness for providers, and new hospital funding models could help stabilize rural maternity services.
How are rural communities responding to maternity ward closures?
Some are turning to mobile clinics, telehealth, and regional hospital partnerships to bring care closer, though these can’t fully replace local wards.
What is the maternal mortality rate in the U.S. compared to other countries?
The U.S. has the highest maternal mortality rate among wealthy nations—nearly three times higher than Canada and the U.K.—with limited maternity access as a key factor.
Read More: “The Importance of Comfortable and Quality Seating in Labor and Delivery Rooms”
Champion’s Commitment to Maternal Health
The future of labor and delivery in the U.S. will depend on collaboration among policymakers, providers, and communities to close gaps in care. At Champion Healthcare Solutions, we believe part of that future also means ensuring mothers have comfort and support during labor, delivery, and recovery.
That’s why we designed the Augustine. Built with a person-centric approach, the Augustine medical recliner combines clinical durability with the look and feel of home furnishings. Its enhanced range of motion allows patients to select positions that promote independence and relaxation, while a spacious seat ensures comfort during long stays.

Ready to explore how the Augustine or another Champion medical recliner can support your labor and delivery unit? Build your chair today with our virtual configurator. Then, connect with our team to ensure it’s the right solution for your facility.
