Professional healthcare clinicians know the impact dialysis treatments can have on their patients. But these experts don’t experience the enormous toll caregiving exacts from laypeople—kind, big-hearted people who aren’t trained or licensed and whose full-time job is not in the medical field.
This blog aims to highlight some of the most common challenges, share the science and data that reveal the problems, and suggest practical solutions to address the key issues.
The Overlooked Challenges of Informal Caregivers in Dialysis Support
Informal caregivers, often family members or close friends, play a vital yet undervalued role in the lives of individuals undergoing dialysis treatments. While professional healthcare clinicians are highly skilled at managing the medical aspects of dialysis, they may not fully grasp the emotional, physical, and logistical burdens carried by those providing unpaid care. This gap in understanding can lead to missed opportunities to support caregivers, ultimately impacting both their well-being and the quality of care provided to patients.
One of the primary challenges faced by informal caregivers is the emotional toll of caregiving. Watching a loved one endure the rigors of dialysis—frequent visits to the clinic, dietary restrictions, and the physical exhaustion that often accompanies treatment—can be distressing.
Caregivers often internalize this stress, struggling with feelings of helplessness and fear about their loved one’s prognosis. While clinicians focus on patient outcomes, they may not always recognize the deep emotional strain caregivers experience, including the guilt they may feel for prioritizing their own needs.
Sign up to get the latest industry news and offers right in your inbox
The physical demands of caregiving also go underappreciated. Many caregivers take on tasks such as assisting with transportation to dialysis centers, helping with meal preparation to meet dietary restrictions, and providing hands-on care during recovery periods. These responsibilities often compound the caregiver’s existing workload, particularly for those balancing full-time jobs or raising children. Healthcare professionals may assume that caregivers have the bandwidth to handle these additional tasks, underestimating how physically draining and time-consuming they can be.
Dialysis treatments are not only costly but also necessitate frequent travel, time off work, and potentially hiring additional help for other household responsibilities. Informal caregivers may face increased financial insecurity as they redirect resources to support their loved one’s care. Clinicians focused on treatment plans and medical outcomes may not realize the extent of the financial sacrifices being made behind the scenes, which can amplify stress and feelings of burnout.
Perhaps one of the most significant gaps in understanding lies in the lack of acknowledgment of caregivers’ mental health needs. Depression, anxiety, and burnout are prevalent among informal caregivers, yet these issues are rarely addressed during clinical visits.
Caregivers often feel invisible within the healthcare system, with their concerns relegated to the background as clinicians prioritize the patient. This oversight not only undermines caregiver well-being but can also negatively affect the patient, as a struggling caregiver may be less able to provide consistent, high-quality support.
Science Shows How Profoundly Patients’ Dialysis Treatments Can Impact Their Caregivers
Beginning dialysis profoundly affects patients and their informal caregivers, with patients often experiencing reduced health-related quality of life (HRQoL) and significant symptom burdens. These challenges create a heavy reliance on informal caregivers, whose own quality of life may also decline due to increased responsibilities and lifestyle changes, potentially affecting the patient’s well-being.
Research indicates that at the start of dialysis, over one-third of caregivers face moderate to high levels of burden, with their mental and physical HRQoL slightly lower than the general population. Patients’ lower mental HRQoL and severe symptoms correlate with higher caregiver burden and reduced caregiver mental HRQoL. However, caregivers’ physical health outcomes seem less influenced by their caregiving role.
The findings highlight the need for integrated support for both dialysis patients and their caregivers, as their experiences are interconnected. Healthcare providers should acknowledge caregivers’ crucial role and address the challenges they face. Further research is essential to better understand and reduce caregiver burden, including studies exploring causality, bidirectional effects, and strategies tailored to the needs of patients and caregivers alike.
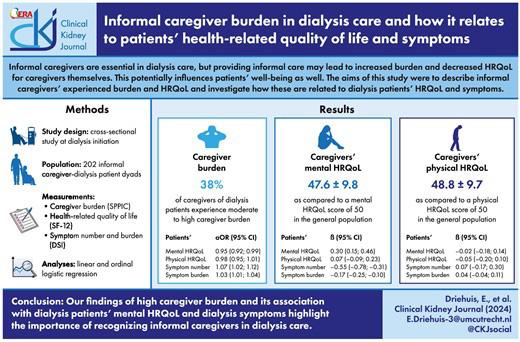
Read More: “Informal caregiver burden in dialysis care and how it relates to patients’ health-related quality of life and symptoms” – Clinical Kidney Journal
By fostering a more holistic understanding of the caregiving experience, clinicians can ensure that informal caregivers feel seen, supported, and equipped to handle the complex demands of their role.
Caregiving and the Cycle of Support
Knowledge is power, and the more providers know about the issues caregivers face, the more can be done to alleviate the heavy burden. This support will help the caregiver stay healthy and also help improve patient outcomes.

Common Challenges Dialysis Caregivers Face
- Emotional Strain: Coping with the stress of watching a loved one undergo frequent treatments and the uncertainty of their prognosis.
- Physical Demands: Managing transportation, preparing meals, and providing post-treatment care, often on top of other responsibilities.
- Time Constraints: Balancing caregiving with work, parenting, or other obligations, leading to potential burnout.
- Financial Strain: Covering travel expenses, missed workdays, and additional household costs associated with caregiving.
- Mental Health Impact: High rates of depression, anxiety, and feelings of isolation due to the caregiving role.
- Lack of Acknowledgment: Feeling overlooked or undervalued by medical professionals during treatment planning and care discussions.
What Caregivers Want the Medical Team to Understand
- A caregiver’s role is essential but often comes at a personal cost in terms of health, finances, and emotional well-being.
- Caregivers are not medical professionals and may feel overwhelmed by the technical demands of caregiving.
- Caregiver insight and observations about the patient’s condition at home can be invaluable.
- Caregivers need acknowledgment and support to remain effective and prevent burnout.
Practical Steps Healthcare Providers Can Take to Address Caregiver Challenges
- Acknowledge Their Role: Regularly recognize and validate the contributions of caregivers during appointments.
- Provide Education: Offer clear, simple guidance on managing post-treatment care, dietary needs, and recognizing warning signs.
- Encourage Self-Care: Suggest local caregiver support groups, counseling services, or respite care options.
- Communicate Openly: Include caregivers in treatment discussions and encourage them to ask questions.
- Offer Resources: Provide information on financial aid programs, transportation services, and community resources that can ease the burden.
- Screen for Burnout: Ask caregivers about their mental and physical health and refer them to appropriate resources when necessary.
- Be Flexible: Accommodate scheduling needs where possible to minimize disruptions to caregivers’ lives.
By addressing these challenges and incorporating caregivers into the care plan, medical teams can help ensure better outcomes for both the patient and their support system.
Enhanced Comfort and Care for Infusion Treatments
Also available in wingback style, the Ascent from Champion Healthcare Solutions features extra padding for patient comfort during treatment, subtle curves for a modern aesthetic, and swing-away arms for easier ingress and egress. With the durable engineering and strength of the Classic but with an upscale design, the Ascent is an ideal medical chair for patients and providers and is commonly used in dialysis, infusion, and oncology settings.
Fast Facts:
 Designed for Durability: With a reinforced steel powder-coated frame and heavy-duty casters, the Ascent medical recliner is built to last.
Designed for Durability: With a reinforced steel powder-coated frame and heavy-duty casters, the Ascent medical recliner is built to last.- Higher Weight Capacity Option: Engineered to accommodate patients up to 500 pounds, the bariatric model (XL, 66P) is deeper and wider than the standard model.
- Quality That Counts: For quality engineering and patient-centric innovation that prioritizes functionality, safety, and comfort, Champion products comply with ISO 13485 and are made in the USA.
To view Champion’s entire portfolio of products, browse our digital catalog. Then, request a quote for your facility.
