Nursing is demanding across every specialty, but in oncology, the pressures are magnified. Oncology nurses face challenges that ripple through entire treatment centers—impacting retention, patient satisfaction, compliance, and financial performance.
For decision-makers, understanding these challenges is essential to creating a sustainable care environment that supports both staff and patients.
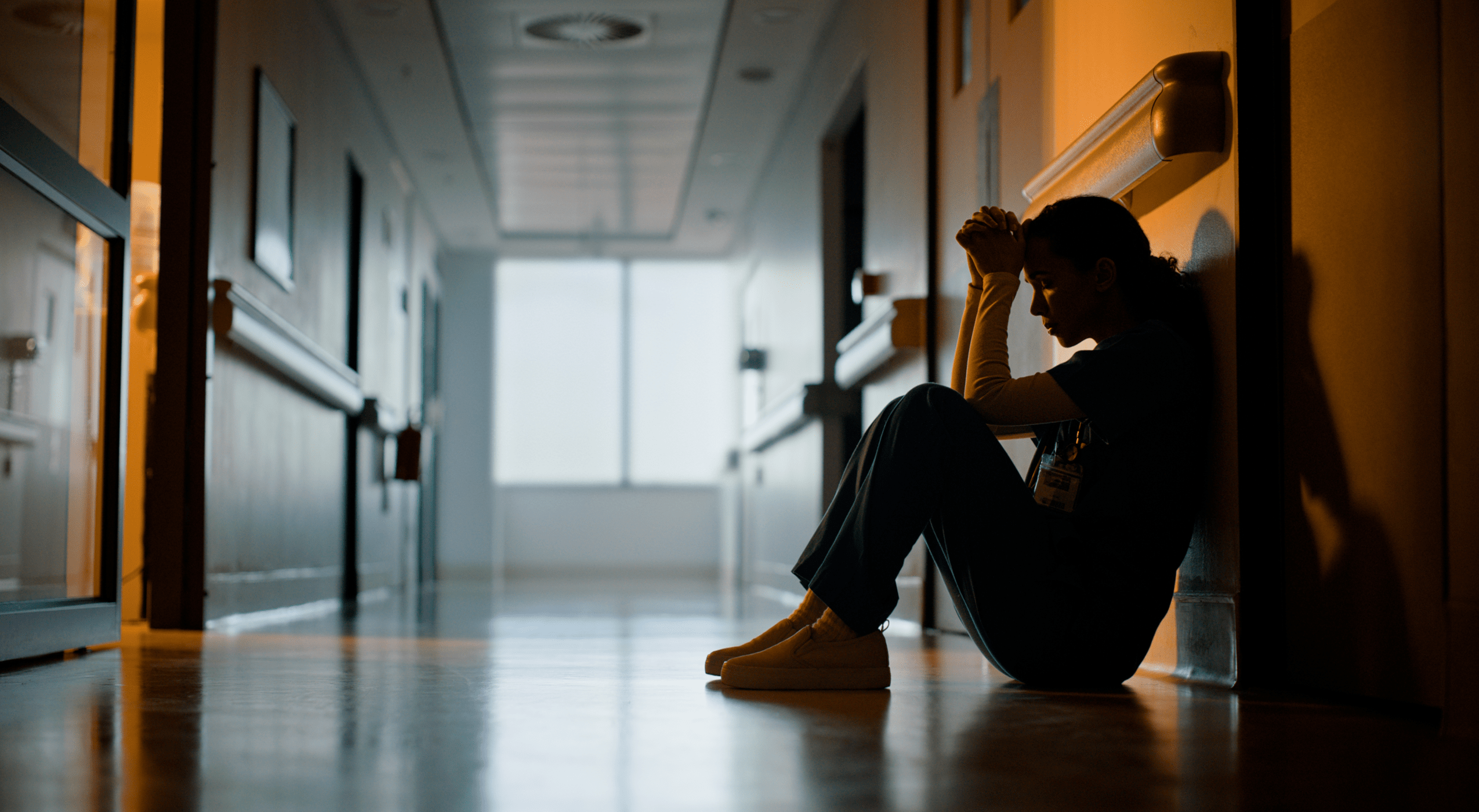
The Emotional Weight of Cancer Care
Oncology nurses form long-term relationships with patients undergoing months or years of treatment. That closeness brings rewards, but also a heightened emotional toll.
- A meta-analysis of nearly 10,000 oncology nurses found 30% experience emotional exhaustion and 35% report a low sense of personal accomplishment—two hallmarks of burnout (BMC Nursing).
- Among hematology/oncology nurse practitioners, over 31% reported burnout and nearly 22% expressed intention to leave the field (NIH).
For administrators, this isn’t just a wellness concern—it’s an operational one. Burnout fuels turnover, turnover drives recruitment costs, and constant onboarding disrupts continuity of care.
Sign up to get the latest industry news and offers right in your inbox
Technical Complexity and Safety Risks
Oncology nurses administer some of the most complex therapies in healthcare, from chemotherapy to immunotherapy. These treatments require precise handling and constant monitoring for life-threatening complications like infusion reactions or neutropenia.
They also face safety risks unique to their specialty. Hazardous drugs are a well-documented occupational hazard:
- A study of 12 infusion centers reported 61 hazardous drug spills among 51 nurses, with some spills as large as 250 mL (NIH).
- Despite protective equipment, surface contamination remains a persistent issue in infusion clinics (CDC/NIOSH).
For leaders, safety concerns translate into regulatory compliance pressure under USP <800>, as well as liability and workforce retention risks.
Physical Demands in Infusion Settings
Unlike specialties with short patient encounters, oncology nurses often spend hours monitoring each patient during infusions. This creates unique ergonomic demands.
- Patients may remain in recliners for four to six hours at a time, requiring frequent adjustments of IV lines and positioning.
- Over time, these repetitive tasks can increase musculoskeletal strain and injury risk.
According to the UKG Workforce Institute, 42% of nurses report skipping breaks during shifts, a factor that contributes to fatigue and error risk.
For administrators, ergonomic strain isn’t just a wellness issue—it’s tied to workers’ compensation claims, absenteeism, and lost productivity.
Read More: “Creating a Culture of Care Starts in the Break Room”
Navigating Family Dynamics
Cancer care rarely involves only the patient. Oncology nurses spend significant time educating and supporting families, answering questions, and guiding them through difficult decisions.
This emotional labor is demanding for staff, but also central to patient experience scores, which increasingly affect reimbursement and reputation.
Why It Matters—and What Leaders Can Do
Every challenge oncology nurses face carries organizational consequences:
- Burnout and emotional fatigue → higher turnover, recruitment costs, and disruptions in care continuity
- Hazardous drug exposure → compliance risks under USP <800>, liability, and long-term workforce health concerns
- Ergonomic strain → staff injuries, absenteeism, and reduced productivity
- Family dynamics → additional staff workload, but also direct influence on patient satisfaction and reimbursement

For administrators, the solution isn’t only acknowledging these risks—it’s acting on them:
- Audit burnout and retention metrics to spot early warning signs.
- Strengthen compliance by ensuring USP <800> standards are fully implemented.
- Evaluate ergonomic conditions in infusion spaces—chairs, layout, and workflow.
- Engage nurses in decision-making about equipment and workflow—they know the pressure points firsthand.
By connecting nurse well-being with organizational outcomes, leaders can create environments that protect staff, satisfy patients, and safeguard financial performance.
A Human Example
Consider a nurse working back-to-back infusion sessions. The patient is in a recliner that sits too high for IV access, forcing awkward bending. The fixed armrest makes repositioning difficult. After multiple patients, the nurse’s back aches, their pace slows, and their patience wanes.
Multiply that across an entire staff, day after day, and the impact becomes clear: lower morale, reduced efficiency, and higher turnover. For leadership, equipment decisions ripple outward into retention, compliance, and patient experience.
Supporting Nurses with the Right Tools: The Alō Recovery Recliner
At Champion Healthcare Solutions, we believe equipment must support both patients and providers. In oncology and infusion settings, seating is not just furniture—it’s a frontline tool that shapes safety, efficiency, and satisfaction.
The Alō Recovery medical recliner was designed for this environment:
- Lower working height to reduce ergonomic strain and ease patient transfers
- Infinite recline positions and swing-away arms for comfort and clinical access
- Durable, all-steel modular frame built for heavy daily use in high-volume centers
- Options like USB charging, heat and massage, and fold-away tables to improve patient experience and streamline staff workflows

By investing in recliners that support both patient rest and nurse workflow, leaders can reduce strain, improve satisfaction, and strengthen compliance.
Ready to Upgrade Your Oncology Environment?
Try our virtual configurator to design a custom medical recliner for your facility, or contact our team to learn how Champion seating can support both your staff and patients.
